Diabetes mellitus is a group of metabolic diseases characterized by high levels of glucose ("sugar") in the blood.
Why do we need glucose
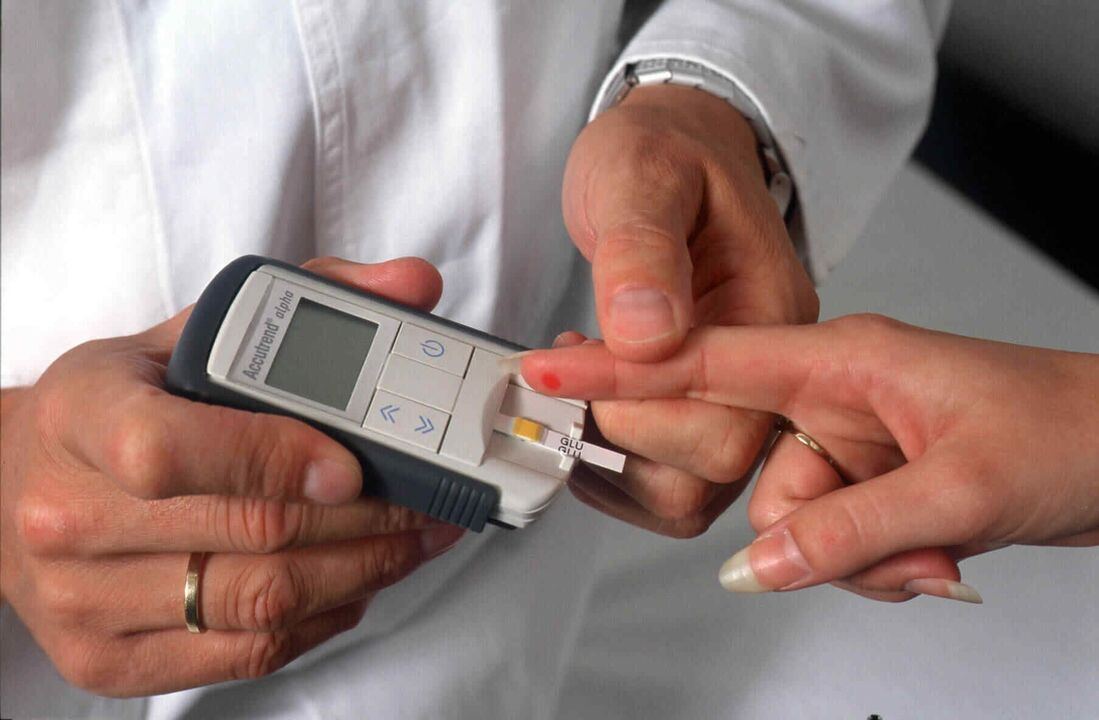
The norm of blood glucose (sugar) in whole capillary blood is 3. 3-5. 5 mmol/l in the morning on an empty stomach (i. e. after 7-14 hours of overnight fasting) and up to 7. 8 mmol/l after meals (i. e. 1. 5 -2 hours after the last meal).
Normally, in the human body, glucose is used by the cell as a source of energy (that is, the body's cells "feed" on glucose from the blood). The harder a cell works, the more energy (glucose) it requires.
Glucose (the expression "blood sugar" is more often used, but this is not entirely true) constantly circulates in human blood. There are 2 ways for glucose to enter the human body: - the first is through foods containing carbohydrates, - the second is through the production of glucose by the liver (this is why in diabetes mellitus, even if the patient has not eaten anything, the blood glucose level may be increased).
However, to be used for energy, glucose from the blood must go to the muscles (to do work), adipose tissue, or the liver (the body's glucose storage site). This occurs under the influence of the hormone insulin, produced by the beta cells of the pancreas. As soon as the blood glucose level rises after a meal, the pancreas instantly releases insulin into the blood, which, in turn, binds to insulin receptors in muscle, fat or liver cells. Insulin, like a key, "opens" the cells to allow glucose to enter them, bringing the blood glucose (sugar) level back to normal. Between meals and at night if necessary, glucose enters the blood from the liver store, so at night insulin controls the liver so that it does not release too much glucose into the blood.
If a violation occurs at any stage of this process, diabetes mellitus occurs.
Types of diabetes
Type 1 diabetes mellitus (previously used name: insulin-dependent diabetes mellitus) develops mainly at a young age (usually before the age of 30, although type 1 diabetes mellitus can also develop at an older age).
Type 1 diabetes mellitus is caused by the cessation of insulin production by the pancreas due to the death of β cells (responsible for insulin production in the pancreas). The development of type 1 diabetes mellitus occurs against the background of a special genetic predisposition (that is, a person was born with it), which, when exposed to some external factors (for example, viruses), leads to a change in the state of the immune systemof the body. The body of a patient with type 1 diabetes begins to perceive his pancreatic β-cells as foreign and protects itself from them by producing antibodies (similar to what happens when protecting against infections), leading to the death of the pancreatic β-cells, which means severe insulin insufficiency.
Diabetes mellitus 1 The type develops when at least 90% of the β cells in the pancreas die. Let us remember the mechanism of action of insulin, its function as a "key" that opens cells to sugar. In type 1 diabetes mellitus, this key has disappeared from the blood (see figure).
Lack of insulin in type 1 diabetes mellitus The onset of type 1 diabetes mellitus is acute, always accompanied by severe symptoms of hyperglycemia (high blood sugar level): - weight loss (the patient loses weight involuntarily), - constant feeling ofhunger, - thirst, dry mouth (the patient drinks a lot of fluids, including at night), - frequent urination (in regular or large portions, including at night), - weakness.
If you do not consult a doctor in time and do not start treating type 1 diabetes with insulin, the condition worsens and a diabetic coma often occurs.
Type 2 diabetes mellitus (previously called insulin-dependent diabetes mellitus) is much more common than type 1 diabetes mellitus. The incidence of type 2 diabetes mellitus is typical of the elderly: it is detected, as a rule, from the age of 40, although recently, according toWHO experts, the average age of patients with type 2 diabetes mellitus is increasingly younger.
About 80% of people with type 2 diabetes are overweight. In addition, type 2 diabetes is characterized by heredity - high prevalence among close relatives.
In type 2 diabetes, the pancreas continues to produce insulin, often in larger amounts than usual. Although there are also cases of type 2 diabetes mellitus with reduced insulin secretion.
The main defect in type 2 diabetes is that the cells do not "feel" insulin well, that is, they do not open well in response to interaction with it, so that blood sugar cannot fully penetrate inside (see figure). level remains high. This state of decreased insulin sensitivity is called insulin resistance.
Low insulin sensitivity in type 2 diabetes mellitus You can figuratively imagine that the "keyholes" (scientifically speaking - insulin receptors) in the cell doors are deformed and there is no perfect match with the keys - insulin molecules. It takes more effort (more keys, i. e. more insulin) to overcome the defect in the insulin receptor. The pancreas cannot supply a sufficient amount of insulin to the blood to overcome insulin resistance and completely normalize blood sugar levels, becauseIn type 2 diabetes mellitus, the capabilities of β cells are still limited.
As a result, in type 2 diabetes, a paradoxical situation arises when there is too much insulin and sugar in the blood at the same time.
Type 2 diabetes mellitus, unlike type 1 diabetes mellitus, begins gradually, often completely unnoticed by the patient. Therefore, a person can be sick for a long time, but not know it. High blood sugar (glucose) levels may be detected by chance during a test for some other reason.
At the same time, there are cases with clear manifestations of hyperglycemia:
- weakness, fatigue, thirst, dry mouth (the patient drinks a lot of fluids, including at night),
- frequent urination (regular or in large quantities, including at night),
- itchy skin (especially in the perineal area),
- slow wound healing, - frequent infections, - blurred vision.
Diabetic coma develops much less frequently, usually if type 2 diabetes mellitus is accompanied by some other very serious illness: pneumonia, serious injury, suppurative processes, heart attack, etc.
Diabetes treatment
Treatment for diabetes differs depending on the type of diabetes.
In type 1 diabetes mellitus, which occurs as a result of an absolute insufficiency of insulin secretion by the pancreas itself, constant self-monitoring and insulin treatment are necessary to preserve life. It should be emphasized that treatment with externally administered insulin is the only treatment option in this situation. The selection of doses and regimens for treating diabetes mellitus with insulin is carried out individually, taking into account age, gender, physical activity and individual sensitivity to insulin.
For type 1 diabetes mellitus Sometimes, at the very beginning of the disease, after the normalization of blood glucose levels during the treatment of diabetes mellitus with insulin, the need for it suddenly begins to decrease until it is completely canceled. But this is not recovery. This phenomenon is called the diabetes "honeymoon", or scientifically, remission. This is explained by the fact that after normalizing blood sugar with the help of insulin, β-cells that have not yet died can function for some time. Afterwards, everyone dies and the person needs treatment for diabetes mellitus with insulin for the rest of their life. Anyone who develops type 1 diabetes for the first time should be warned by their doctor about the possible occurrence of such a situation and what to do in this case.
Treatment of diabetes mellitus with insulin can be carried out using insulin syringes, pens or an insulin pump.
Insulin pump therapy is an alternative treatment for diabetes in people who heavily use a syringe or pen to inject insulin and regularly measure their blood sugar levels. Insulin pump therapy is used instead of treating diabetes with injections. The pump is worn on the body or on clothing, for example on a belt. Currently, around 250, 000 people around the world use insulin pumps.
The main goal of treating type 2 diabetes is to improve the sensitivity of cells to insulin. The causes of low insulin sensitivity are not yet fully understood. However, it has long been known that the most powerful factor in the formation of insulin resistance is excess weight, that is, excessive accumulation of fat in the body. Numerous scientific studies and long-term observations of patients show that weight loss during the treatment of type 2 diabetes in most patients can achieve a significant improvement in blood sugar levels.
In type 2 diabetes, normalization of weight can lead to complete normalization of blood sugar over a long period, although this cannot be called complete recovery.
If diet and exercise aimed at weight loss do not have enough effect in treating type 2 diabetes, it is necessary to resort to medication. They are available in tablets. Some of them act on the pancreas, increasing insulin production, while others improve its action (reduce insulin resistance). So, the drugs themselves used in the treatment of type 2 diabetes mellitus do not reduce blood sugar, insulin does this, therefore, to obtain the effect of tablets in the treatment of diabetes mellitus, a preserved reserve of pancreatic β-cells is necessary. This makes it clear why it is useless to use tablet medicines in the treatment of type 1 diabetes, because most of the β cells have already died.
Insulin is often used to treat type 2 diabetes. Insulin treatment for type 2 diabetes mellitus may be prescribed as a temporary measure, for example during surgery, severe acute illnesses, or as permanent treatment. This is why it is currently not recommended to call type 2 diabetes mellitus non-insulin dependent. The type of diabetes treatment does not determine the type of diabetes.
Diet plays the most important role in treating diabetes.
Diet for diabetes
Despite the common goals in treating different types of diabetes (eliminating symptoms of high blood sugar levels, minimizing the risk of hypoglycemia, preventing complications), dietary patterns for type 1 and type 2 diabetes mellitus differ significantly. There is no single eating plan for diabetes mellitus.
In type 1 diabetes mellitus, the occurrence of which is associated with the death of beta cells in the pancreas and insulin deficiency, the main method of treatment is insulin replacement therapy, and dietary restrictions, according to the modern view, are of an auxiliary andshould be administered only to the extent that insulin therapy differs from insulin production in a healthy person.
The fundamental principles of diet prescription for type 1 diabetes mellitus have been the subject of critical review in recent years.
One of the principles of the traditional diabetes diet is the recommendation to consume an identical and strictly defined amount of calories daily. Each patient received a daily caloric prescription based on "ideal weight. "This makes no sense and is impossible for the following reasons:
- In healthy individuals with normal weight, the balance between energy intake and expenditure varies greatly from one day to the next. Energy expenditure in healthy individuals is variable because their physical activity is variable. Consequently, if you prescribe a patient with type 1 diabetes a certain diet with a daily consumption of a fixed and identical amount of calories, then to maintain a normal weight you will have to recommend an equally strict plan of physical activity. for every day, which is absolutely unrealistic.
- In patients with type 1 diabetes mellitus with normal weight and an appropriately selected insulin treatment regimen for diabetes mellitus, appetite regulation does not differ from that in healthy individuals. The fact that they sometimes have to be forced to eat to prevent hypoglycemia, even in the absence of appetite, is most often a consequence of not entirely adequate insulin therapy.
Improved diabetes mellitus treatment regimens with insulin and self-monitoring of metabolism based on blood sugar levels give the patient the opportunity to regulate food intake solely depending on the feeling of hunger and satiety, like healthy people. Thus, the diet of a patient with type 1 diabetes mellitus corresponds to a complete healthy diet (balanced in calories and content of essential nutrients). The only difference is that injected insulin doesn't "know" when or how much you eat. Therefore, you yourself must ensure that the insulin action corresponds to your diet. Therefore, you need to know which foods increase blood sugar.
The main method of treating type 2 diabetes is normalizing body weight through a low-calorie diet and increased physical activity. Diet for type 2 diabetes is very important; It is one of the important components that allows you to achieve success.
All food products consist of three components: proteins, fats and carbohydrates. They all contain calories, but not all of them raise blood sugar.
Only carbohydrates have a pronounced blood sugar-raising effect. What foods contain carbohydrates? It's easy to remember: most of the products are of plant origin, and of animal origin - only liquid dairy products. It's important that you know whether your blood sugar rises after certain foods and, if so, by how much. There are types of carbohydrate foods, after which blood sugar does not rise or rises only slightly.
All carbohydrates can be roughly divided into two groups: those containing quickly absorbed ("fast") carbohydrates and slowly absorbed ("slow") carbohydrates. "Fast" carbohydrate products contain refined sugars and include preserves and jellies, candies, sweets, fruits and fruit juices. "Fast" carbohydrates cause a sharp rise in blood sugar (depending on the amount of food eaten) because they are quickly absorbed into the blood, so it is best to exclude them from the diabetes diet. "Slow" carbohydrates are much more beneficial for diabetes patients because they take much longer to be absorbed. Furthermore, the absorption of sugars is delayed by the fiber contained in food, which is why the diet in the treatment of diabetes must be enriched with foods rich in fiber.
Here are some simple rules to follow when treating diabetes: food should be eaten in small portions and frequently (4-6 times a day); follow the established diet - try not to skip meals; do not overeat - eat as much as recommended by your doctor; use bread made with wholemeal flour or bran; vegetables (except potatoes and legumes) should be consumed daily; Avoid eating "fast" carbohydrates.
Exercise for Diabetes Physical exercise in the treatment of diabetes is very important: it increases the sensitivity of the body's tissues to insulin and thus helps reduce blood sugar levels.
Housework, walking and running can be considered physical activities. Preference should be given to regular and dosed physical exercise: sudden and intense exercise can cause problems in maintaining normal sugar levels.
If you are an athlete or sportsperson, you have no contraindications to practicing sports, as long as your blood sugar levels are well controlled and all necessary measures are taken to prevent their significant decrease.
Preventing Diabetes Complications Patients with diabetes have an increased risk of developing heart and blood vessel complications (especially in the legs and kidneys). Regular physical activity, sometimes just walking, is enough to prevent circulatory problems in the feet.
If you have diabetes, an untreated wound or abrasion on your foot can turn into a serious problem. Even small cuts or scrapes on the feet take longer to heal than in patients without diabetes and require greater attention. The key to preventing these problems is to wear well-fitting shoes and check your feet frequently. Use a mirror if you find it difficult to examine all areas of your feet, and remember that foot injuries are often painless at first and can go unnoticed for a long time if you are not careful enough.
Patients with diabetes are at increased risk of kidney dysfunction and heart disease several years after diagnosis. There is good evidence that good blood sugar control reduces this risk. In addition, to prevent complications from diabetes mellitus, it is necessary to undergo preventive treatment twice a year.
Blood pressure control is also important. Check your blood pressure regularly. If it is elevated, your doctor will prescribe treatment for you.

























